At 36, Adam Wereszczynski was gobsmacked when tests revealed he had liver disease.
As a finance professional, long workdays spent crunching numbers and evenings dedicated to client entertainment left little time to think about his health.
Now aged 42, he told the Daily Mail: ‘I was slightly overweight, but I was going for runs and going to the gym when I could. I was tired all the time, but I just put that down to how busy I was. I never even thought twice about my liver – but when you’re young, you do tend to think you’re a bit invincible.’
At the time, Adam was eating out at least five nights a week, either at business dinners or with his partner, and admits he was partial to rich dishes.
He said: ‘When you’re entertaining clients, you tend to go to some of London‘s best restaurants – and the food tends to be more decadent.’
While he didn’t drink to excess, he would have a couple of glasses of red wine with a meal, and although he’s ‘never been a pub person’, he also enjoyed sharing a good bottle with friends while socialising.
He added: ‘The nights I wasn’t having dinner at restaurants, I’d often finish late and order a takeaway, but in hindsight, even though I thought I was making healthy choices, I was totally uneducated about how much hidden fat I was eating. I wouldn’t be ordering fish and chips or anything like that. I prefer Asian food, but I didn’t consider that the sauces were very heavy, very fatty.’
It was after a random dinner party conversation about hangovers that Adam was inspired to look more closely at his liver health.

Adam Wereszczynski was gobsmacked when tests revealed he had liver disease
‘I was complaining about how lethargic hangovers left me, and how tired I felt overall, when someone suggested it might be to do with my liver.’
Although Adam had private healthcare, and regular screenings found him to be in ‘good health, apart from a high-ish BMI,’ he decided to heed the stranger’s advice and booked a scan at The Liver Clinic in London.
At that same appointment, he was diagnosed with a form of liver disease known as non-alcoholic fatty liver disease (NAFLD), also referred to as metabolic dysfunction-associated steatotic liver disease (MASLD). This condition is becoming increasingly common.
‘It was a bit of a shock. I wasn’t expecting it, purely because all the health checks I’d had seemed to suggest that I was absolutely fine,’ he said.
‘I used to play rugby so I’m always going to be a bit bulky and have a higher BMI, but I never expected to be told that my liver was full of fat.’
Adam isn’t alone in having a liver hiding a silent potential killer. The British Liver Trust estimates that one in five people have MASLD, making it the most common form of liver disease in the UK, affecting 15million people.
Its symptom-less nature is one of the main reasons experts are so concerned about the surge in cases.
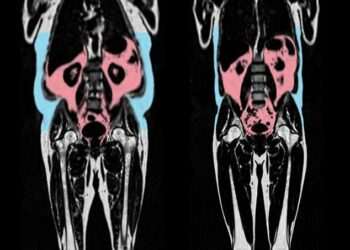
MASLD occurs when fat builds up inside the liver, disrupting its functions and triggering inflammation. Over time, this leads to scarring, which can eventually cause cirrhosis – putting the liver at risk of failure. It is also known to be a precursor to deadly liver cancer.

It’s a common and dangerous misconception that only alcohol can cause liver scarring
Figures from The Liver Trust revealed that there were 11,000 deaths from liver disease in 2024 – and many of these could have been avoided with early intervention and lifestyle changes.
Adam wants to share his story to encourage others to take their liver health seriously.
Professor Philip Newsome, Director of the Roger Williams Institute of Liver Studies at King’s College London, explains: ‘People who develop MASLD are often overweight or have diabetes. We’re seeing an increase in liver disease in the UK, and the challenge is that symptoms are often not noticeable until it’s too late.’
He adds that it’s a common and dangerous misconception that only alcohol can cause liver scarring, as excess fat can lead to the same outcome.
‘As fat accumulates, it can damage the cells inside the liver, resulting in inflammation, irritation, and, in some cases, internal scarring,’ he said.
‘Over time, this can develop into liver cirrhosis, which is a very advanced stage of scarring.’
Around a third of people have increased fat inside their liver, but the good news is that only about one per cent will develop internal scarring. However, severe metabolic challenges – such as diabetes, high cholesterol, high blood pressure, or higher weight – can increase the likelihood of scarring.
As Britons’ waistbands continue to strain under the weight of an obesity crisis, more people are at risk of developing MASLD – or are already unknowingly living with it.

The lack of symptoms in the early stages is one of the main reasons experts are so concerned about the surge in cases
Dr Gareth Morris-Stiff, a surgical oncologist with decades of experience treating liver, pancreas, and biliary tree tumours, describes the liver as the ‘master regulator of the body’.
He told the Daily Mail: ‘Everything you take into your body, be it food, drink, medications – anything – your liver will metabolise it.
‘It’s exposed to everything you ingest, plus everything you produce internally that enters the blood, including hormones. It regulates fats, proteins, carbohydrates, vitamins.
‘Everything is processed through the liver – it has at least 500 vital functions and thousands of enzymatic processes.’
With the rise of ultra-processed foods (UPFs), chemicals and pesticides in the food chain, and increasing concerns about microplastics – plus more sedentary lifestyles and air pollution – our livers are facing growing challenges.
Dr Morris-Stiff agrees that diet is the main culprit putting stress on our livers.
‘For most people, the biggest damaging factor is the consumption of ultra-processed foods, which are ubiquitous in the Western world. Artificial sweeteners are also a problem, as the liver doesn’t metabolise them the same way it does sugar, making them difficult to process.’
Similarly, when we consume artificial chemicals – such as dyes, colorings, and sugars – the liver struggles to process them, triggering inflammation. This leads to fat deposition, which becomes inflamed and progresses to scarring, fibrosis, cirrhosis, and potentially cancer.

Follow-up tests revealed that the fat levels in Adam’s liver had returned to healthy levels, and they remain normal after maintaining his healthier lifestyle
But even a plant-based diet doesn’t guarantee protection, according to Dr. Morris-Stiff.
‘Even vegetables can be a threat because they’re often sprayed with chemicals and fertilisers. Unless you have high-quality vegetables and wash them thoroughly, you’re at risk, even if you predominantly eat vegetables.’
If left untreated, MASLD can lead to liver cirrhosis, which is closely linked to the development of primary liver cancer – a ‘silent’ killer, according to leading oncologist Dr Anya Adair.
‘When it comes to liver cancer, prevention is obviously better than cure,’ she said. ‘If we can’t prevent it, we need to catch it early – but that’s difficult, as it’s a silent cancer.’
Dr Adair explains that symptoms of liver disease, including MASLD, often mask the presence of liver cancer.
‘People don’t usually present symptoms until it’s very advanced, and often it develops in the background of cirrhotic liver disease,’ she said.
Once seen as a disease affecting mainly older people with hepatitis infections or alcohol dependency, liver cancer – particularly hepatocellular carcinoma (HCC) – is now increasingly diagnosed in people in their 30s and 40s.
A major new analysis published in The Lancet predicts that liver cancer cases worldwide will rise from 870,000 in 2022 to 1.52 million by 2050, with annual deaths increasing from 760,000 to 1.37million over the same period.
Experts say the fastest-growing cause of liver cancer is MASH (metabolic dysfunction-associated steatohepatitis), an advanced stage of MASLD. The proportion of liver cancers linked to MASH is expected to more than double, from 5 per cent in 2022 to 11 per cent by 2050.
The number of cases caused by hepatitis B and C is expected to decline.
Professor Newsome says: ‘Cirrhosis can take 20 to 40 years to develop, during which time the liver continuously tries to regenerate. Sometimes, this attempt to regenerate becomes pathological, leading to cancerous growths.’
After discovering his hidden condition, Adam made a series of lifestyle changes, including taking a herbal supplement called Deliverance. After several months, he lost two stone.
Follow-up tests at The Liver Clinic revealed that the fat levels in his liver had returned to healthy levels, and they remain normal after maintaining his healthier lifestyle – now focusing on grilled fish and salads over carb-laden starters.
He said: ‘Since getting my liver back to normal levels, I feel a lot more energised than I did before. Even my appearance has changed; people always compliment my skin. I just look healthier than I did before.’