We’ve all been there. Just as you’re peacefully drifting off to sleep, a rattling, rasping snore from the other side of the bed jolts you wide awake.
You prod your other half, to no avail. With a forceful shove they may wake and apologise but, as soon as they drop off, the bone-rattling cacophony resumes.
It’s estimated that 15 million snorers in the UK regularly disturb the peace of the night – and that of their bed partners – with unwelcome noises ranging from mild snuffling to the truly thunderous.
While the popular image of a middle-aged overweight male snorer holds true, in fact, many women also snore, particularly after the menopause – and almost everyone snores at some point.

Writer Judith Keeling reveals that there is plenty of lifestyle advice and gadgets to help people who snore and live with sleep apnoea
The most common age is in midlife (between 30 and 60), partly as this is a time when extra weight creeps on – a major cause – or other lifestyle factors play a role (more on these later).
But as well as being a source of embarrassment and domestic dispute, snoring may also spell a serious health problem.
While snoring can be caused by vibrations of the tissue in the airways – worsened by congestion of some description, such as a blocked nose, for instance – for millions it can also be a sign of obstructive sleep apnoea (OSA), a condition where your airways briefly collapses.
This is where you temporarily stop breathing, cutting off the supply of oxygen. Untreated, sleep apnoea can raise blood pressure and increase the risk of heart attack, stroke, type 2 diabetes and dementia, thought to be largely because of the reduced oxygen supply.
The good news is that there’s plenty of lifestyle advice and gadgets to help people who snore and live with sleep apnoea.
Today, in the first part of our series of essential guides to tackle common ailments – back pain, coughs, dental problems and, here, snoring – we’ve joined forces with leading experts to reveal the ultimate guide to beating your snoring (or that of a loved one), based on the latest scientific evidence, so you can finally get a good night’s sleep…
What’s causing all that noise?
When you sleep, the soft tissues of your tongue, mouth and throat relax, narrowing the airways. As air is forced through this narrowed airway with each breath, it causes this tissue to vibrate, which is what causes characteristic snoring sounds.

Follow this ultimate guide to beating your snoring (or that of a loved one), based on the latest scientific evidence, so you can finally get a good night’s sleep…
A number of factors can worsen snoring.
Simply sleeping on your back makes it more likely that you’ll snore as this position makes the muscles at the back of your throat relax, which can impede the flow of air.
It may also be lifestyle-related, such as drinking alcohol or taking sedatives, as these can both cause the tissues at the back of your throat to relax and partly block the airflow.
Being overweight can contribute too, as the extra fat around the neck presses on the airway while you are lying down, narrowing it further. It can also be related to an anatomical problem, such as large tonsils or a deviated septum (where the wall of cartilage between the nostrils is misaligned).
For women, dwindling levels of oestrogen after menopause can lead to the throat muscles and soft tissues thinning and drying out, making them more prone to vibrating.
Meanwhile, if your nasal passages are blocked due to congestion caused by a cold, flu or an allergy, this can also contribute. And sometimes snoring is a symptom of sleep apnoea.
Adam Frosh, a consultant ear, nose and throat surgeon at East and North Hertfordshire NHS Trust, says there’s a symphony of snoring noises out there, depending on which soft tissue is vibrating.
For example, if it comes from your nose, it produces a whistle sound; throat snoring often leads to a rasping, rattling noise; if it’s the tongue then it’s usually high-pitched; and you sometimes hear a popping noise from the lips and mouth.
‘The main cause of snoring involves a combination of vibrations from the soft palate [the curtain of thin muscles and tissue you can see at the back of the throat], the tonsils and the uvula [the little hanging ball at the back of your throat],’ explains Mr Frosh.
Less commonly, it happens when the base of the tongue vibrates at the back of the throat as air passes over it.
The loudness of the snore does not necessarily correlate to the severity of a problem, however. Steven Frampton, a consultant ear, nose and throat surgeon at University Hospitals Dorset NHS Foundation Trust, explains: ‘Assessing the sound will be only one factor a specialist considers along with a careful detailed examination and visual inspection of nose and throat.’
‘Just’ snoring, or medical problem?
The vast majority of sufferers are ‘simply snorers’. It’s undeniably embarrassing but doesn’t pose long-term health problems. But it can also be a sign of obstructive sleep apnoea (OSA), which affects up to ten million UK adults (many undiagnosed).
In OSA, the muscles and tissue in the throat and neck relax while you’re asleep, blocking the airway and halting the flow of air.

Up to ten million UK adults suffer from sleep apnoea, which can lead to snoring
Once the brain realises breathing has stopped, it sends out a signal for the airway muscles to contract again. This opens the airway, often causing the sufferer to wake with a jolt.
Although OSA can be characterised by a snort or gasp, the sound may not always be different from normal snoring, says Mr Frosh. The key difference is that breathing is interrupted, interfering with the person’s sleep.
‘This can happen many times a night,’ adds Guy Leschziner, a professor of neurology and sleep medicine at Guy’s and St Thomas’s Hospitals in London. The cumulative effect is people with sleep apnoea can feel exhausted the next day and lack concentration. Indeed, sleep apnoea increases the chances of having a car accident two or threefold.
But each brief ‘suffocation’ also causes a rise in heart rate and blood pressure, a stiffening of the arteries and a drop in oxygen levels. Over time, this can raise the risk of high blood pressure, heart attack and stroke.
In addition, sleep apnoea makes you more likely to put on weight – partly because interruptions to sleep interfere with the hormones ghrelin and leptin (which respectively increase or reduce your appetite), and lead to insulin resistance – where your cells stop responding properly to insulin, raising blood sugar levels, a precursor to type 2 diabetes.
There are also dangers for your brain and it is linked to an increased risk of Alzheimer’s disease.
As Professor Leschziner says: ‘One potential explanation is that fragmented sleep disturbs your brain’s waste disposal system – the glymphatic system – which usually clears out toxins and a build-up of the amyloid proteins, linked to Alzheimer’s. But more research is needed.’
The red flag symptoms you should never ignore
A partner may notice if you gasp for air in the night and appear to stop breathing temporarily. But it’s harder to know if you sleep alone.

Even dogs snore so avoid sharing a bed with them if you want to improve the quality of your sleep
Here, Guy Leschziner, a professor of neurology and sleep medicine at Guy’s and St Thomas’s Hospitals in London, shares the red flag signs to watch out for:
- Frequent waking, sometimes gasping or choking.
- Feeling sleepy, even if you think you’ve had a ‘proper’ night’s sleep.
- Going to the loo often at night; especially if you don’t go frequently in the day. Hormone changes caused by interruptions to your sleep can stimulate the kidneys to produce more urine than normal at night.
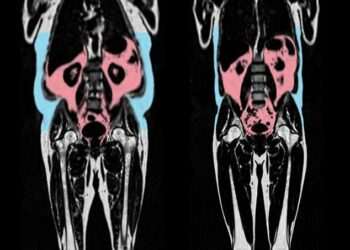
- Being overweight is one of the main risk factors for sleep apnoea. It may be a factor if your neck measures more than 17in (43cm) for a man or 16in (40.5cm) if you are a woman.
- Waking up with a sore throat, dry mouth or a headache. The sore throat and dry mouth is due to vibration of tissue at the back of the throat causing irritation; the headache may be due to changes in blood flow due to lower oxygen levels.
- Vivid dreams – we usually don’t recall dreams, but you may do so if the rapid eye movement (REM) phase has been interrupted.
- Being over 50, if you also have other symptoms. (We tend to put on weight as we age and tissues become less rigid. For women, hormonal changes post-menopause can also contribute.)
- The first port of call should always be your GP.
Seven lifestyle changes that could banish your snoring
1. Roll over
Although heavy snorers will snore in any position, moderate snorers are more likely to snore only when on their back.

Sleeping on your side stops your tongue from falling into your throat, partially blocking your airway
An estimated 10 to 15 per cent of sleepers favour sleeping on their back, but ‘sleeping on your side stops your tongue from falling into your throat, partially blocking your airway’, explains Dr Dipesh Mistry, a consultant psychiatrist and sleep specialist based in London.
He advises placing a heavy pillow behind your back to ensure this.
2. Raise your head
If you’re a back-sleeper, raising the head of your bed by 4 in (around 10 cm) can prevent your head flopping backwards when you sleep. Or buy a wedge-shaped pillow to keep your head more upright.
‘Look for an incline angle of between 30 and 40 degrees,’ suggests Dr Mistry. You may even want to invest in a new gadget that tilts the bed for you (see below).
3. No more night caps
Alcohol relaxes the muscles at the back of your throat.
‘It doesn’t have to be a large amount of alcohol – a glass or two can have this effect, depending on the person, if you have it before bedtime,’ says ear, nose and throat surgeon Steven Frampton.
‘And the more you drink, the greater the likelihood of it causing you to snore.’
In addition, alcohol relaxes the throat muscles sufficiently to induce temporary sleep apnoea in normal snorers, according to the British Snoring and Sleep Apnoea Association – so not only are throat muscles relaxed enough to produce snoring, but they can also temporarily collapse, cutting off breathing – and causing the person to gasp.
4. Use a nasal spray
Whether it’s to treat a seasonal cold or allergy, over-the-counter nose sprays can prove effective.
A quarter of the UK’s population is estimated to have an environmental allergy – ‘these can cause the soft tissue inside the nose to swell, forcing you to breathe through your mouth at night and leading to snoring,’ says Dr Helen Evans-Howells, a GP and allergy specialist based in Poole.
For milder symptoms, non-sedating anti-histamines (e.g. cetirizine or loratadine) can work. But Dr Evans-Howells says that those with severe congestion will need sprays containing corticosteroids to reduce the soft tissue swelling obstructing their airflow.
She advises using sprays to tackle the issue locally rather than oral tablets as potential side-effects include bone thinning if used long-term.
Pirinase (containing fluticasone) is one effective over-the-counter steroid spray, she says.
A GP or specialist may prescribe a treatment such as Dymista that combines an antihistamine with steroids in a nasal spray.
Oral decongestants such as Sudafed, a pseudoephedrine, available over-the-counter might offer immediate relief, but using some decongestants longer than a few days can cause rebound congestion (a worsening of symptoms), adds Dr Evans-Howells.
5. Get a pill review
Tranquilisers, such as Valium, can also relax your throat muscles, making snoring worse.
While sleeping tablets, such as benzodiazepines and ‘Z drugs’ such as zolpidem, may help you to drift off, they also cause throat muscles to slacken, leading to snoring, says Adam Frosh, a consultant ear, nose and throat surgeon based in Hertfordshire.
Always consult your GP before you stop taking any prescription medication.
6. Slim down
Being overweight is a major reason that many people snore, as it often leads to a bigger neck: extra weight here puts pressure on airways. Men tend to have a higher proportion of their body weight around their neck than women – which could be one reason men are more likely to snore.
You’re probably a snorer if your neck measures more than 17 in (43 cm) if you are a man, or 16 in (40.5 cm) if you are a woman. Small changes can help. You may only need to lose 4-5 lb (or 2-3kg) to stop snoring.
7. Quit smoking
Tobacco smoke contains toxins that can irritate the soft palate, causing inflammation, swelling and catarrh.
Even passive smoking can cause inflammation of the nose and throat passages, increasing the chances of snoring – this means children of smoking parents are more likely to snore than children whose parents don’t smoke.
If you can’t quit, at least cut down: the British Snoring and Sleep Apnoea Association advises having your last cigarette four hours before bedtime to give your body time to mitigate the effects.
Should you trust Dr TikTok?
Mouth-taping has become a popular remedy on TikTok for tackling snoring. Videos suggest placing tape vertically across the lips or diagonally across the mouth (in an X-shape) to force you to breathe through your nose.
‘People have been told [by influencers on social media] that if you shut your mouth your tongue is less likely to fall backwards, which is what causes you to snore,’ says Dr Sandip Banerjee, a respiratory and sleep disorders consultant at Medway Maritime Hospital in Kent.
But there is almost no research backing the benefits of mouth taping for snoring, he says – and he’s concerned that for many it may prove unpleasant and even dangerous.

There is almost no research backing the benefits of mouth taping for snoring
‘Taping your mouth shut won’t help someone whose nose is blocked, as they simply won’t be able to breathe properly through their nose. This method will cause anxiety, stress and interfere with their sleep.’
In addition, mouth taping could be ‘dangerous’ for people with severe sleep apnoea, says Dr Banerjee. ‘Just one episode of extra exertion of this nature on their blood pressure can lead to a variable heart rate.’
He adds that obese people also actually need to partly breathe through their mouths as well as their noses – extra fat on your neck, chest and across your abdomen can make it difficult to breathe deeply and may produce hormones that can affect your body’s breathing patterns.
What to eat
Eating a healthy, plant-based diet rich in fruit, veg and wholegrains may help prevent snoring caused by sleep apnoea, according to a study published this year.
And yes, consuming a lot of sugar, refined carbohydrates, starch and salt could put you at greater risk, the researchers from Flinders University in Adelaide, Australia, found.

Eating healthily may help to reduce snoring
The study, which analysed the diets and sleeping patterns of more than 14,000 people, found that those with diets high in fruit, veg and wholegrains were 19 per cent less likely to suffer from sleep apnoea compared with those who consumed more animal fat, dairy, meat, seafood and eggs.
Those who ate unhealthy plant-based diets (including lots of refined carbohydrates such as bread, desserts and salty foods) had a 22 per cent higher risk than people who ate fewer of these ingredients.
It seems the key is that the healthier diets contain antioxidants, fibre and anti-inflammatory compounds, which help weight control and reduce inflammation.
There’s also evidence that eating certain foods – such as poultry, high in the amino acid tryptophan, which plays a role in a healthy sleep-wake cycle and leafy greens and nuts rich in magnesium, which can alleviate stress – can help you get a good night’s rest, adds sleep expert Dr Dipesh Mistry.
Try these two simple tongue exercises
Improving the strength and tone of the muscles of your jaw, tongue and soft palate with daily exercises may reduce both the volume and frequency of snoring, if practised regularly, research shows.

Try this exercise to help prevent snoring: Stick out your tongue as far as you can
A study in the journal Chest in 2015 found that snorers who regularly performed tongue and mouth exercises for three months reduced the volume of their snoring by nearly 60 per cent and the frequency of snoring by 39 per cent.
Exercises target the base of the tongue and the muscles in the upper airway – these can lose tone as we age, as well as relaxing and flopping at night, causing snoring and obstructive sleep apnoea.
Vik Veer, a consultant ear, nose and throat (ENT) surgeon at Royal National ENT Hospital in London, says that exercises can tighten muscles to help prevent them collapsing. He suggests trying the following:
1. Stick your tongue out as far you can – then try to touch your chin or nose. Hold it there for five seconds. Repeat at least three times and up to ten times a day in total.
2. Suck your tongue up to the roof of your mouth. ‘Use your tongue to fill the full surface area,’ says Mr Veer. Hold it for five seconds, then relax. Repeat three times up to a maximum of ten times a day. To increase difficulty, try opening your mouth at the same time.
See Mr Veer’s video: Throat Exercises for Snoring and Sleep Apnoea (myofunctional therapy), via his channel ‘Vik Veer – ENT Surgeon’ on youtube.com
And these herbal remedies
TABLETS and nasal sprays (see above) can help with snoring due to nasal congestion, by helping to open the airways. But some natural remedies can also do this. These include:
- Nasal salt sprays – the salt helps to draw water from the mucous membranes in the nose and open up nasal passages. ‘The treatment also washes out excess mucus, dust, pollution and other allergens,’ says pharmacist Nahim Khan. He recommends Sterimar congestion relief spray (100ml, £8.75, boots.com).
- Essential oils – such as eucalyptus, peppermint and goldenseal – can also be effective, says Nahim Khan – it’s thought they work by relaxing and opening up the airways; they ‘may also have some ability to reduce mucus production’, he says. Menthol, derived from peppermint, also stimulates the cold receptors in the nasal passages, creating a cooling sensation that tricks the brain into perceiving an increased air flow and reduced congestion. Several brands combine menthol and eucalyptus – including Vicks, Olbas Oil and pharmacy own-brand products.
- Eyebright, a flowering plant, is thought to tighten mucosal tissue in the nose and throat, reducing flutter that worsens snoring. It is an ingredient in Rhynil stop snoring spray (35ml, £19.99, britishsnoring.shop).
From masks to tonsil surgery, treatments your doctor can offer
If your efforts to improve your snoring with lifestyle changes have not been successful, there are other effective treatment options.
In general, if you have a nasal obstruction of any description, or have been diagnosed with sleep apnoea, NHS treatments are available.
Otherwise you might consider seeing a specialist privately. Always discuss your options with your GP or other health professional.
Low-tech options gum shield
A simple first step, a mandibular advancement device or splint is a type of gum shield that is useful for people who have mild snoring problems or sleep apnoea, particularly if it’s caused by the tongue falling back and partially blocking the airway.
They are worn over the top and bottom teeth while asleep, to gently push the position of the jaw forward. This opens up the airway, preventing snoring.
You can buy these over-the-counter for around £40. You can get a customised version fitted by a dentist, but these can cost several hundred pounds.
‘I would try the over-the-counter version first to see if this works for you before considering whether you want a custom-made device,’ says Adam Frosh, a consultant ear, nose and throat surgeon in Hertfordshire.
Risks: May cause discomfort around the jaw, drooling and dry mouth. They are generally not suitable for people with epilepsy or for those who wear dentures or who have gum disease.
Oxygen mask
Considered the gold-standard treatment for sleep apnoea, a continuous positive airway pressure (CPAP) machine releases pressurised air to keep your airways open while you sleep.

A continuous positive airway pressure (CPAP) machine releases pressurised air to keep your airways open while you sleep
Users wear a mask that is attached to a bedside device which delivers air at a pressure set by your sleep specialist.
‘Although the machine is highly effective at preventing sleep apnoea, it does take some getting used to,’ says Mr Frosh.
‘As it involves sleeping in a mask, some people may have to train themselves to do this – and some cannot tolerate it.
‘The machine’s whirring may also disturb a partner’s sleep.’
A CPAP machine may not work for someone whose nose is blocked either due to congestion or to an anatomical problem, such as a deviated septum.
Risks: Masks may cause rhinitis, conjunctivitis and skin irritation. A 2004 study found that up to 10 per cent of patients refuse to use their CPAP machine or discontinue use in the first few weeks.
Surgery for sleep apnoea
Surgery is normally offered on the NHS to treat sleep apnoea if CPAP hasn’t worked.
It can also be effective for other causes of snoring, but you will typically have to have this done privately. The main types of surgery that can help are:
Tonsillectomy: Removing enlarged tonsils (that are stopping you breathing properly or causing repeated infections) can significantly improve simple snoring and snoring linked to mild or moderate sleep apnoea.
One 2016 study, published in The Laryngoscope, which looked at patients with moderate obstructive sleep apnoea who underwent a tonsillectomy, found it reduced, on average, breathing interruptions from 40 per night, to just seven.
Risks: Post-operative bleeding and infection (both rare) and voice changes (very rare).
Uvulopalatopharyngoplasty (UPPP): This procedure stops snoring by trimming excess tissue in the soft palate and uvula, which dangles at the back of your throat, stopping them narrowing the airway. Suitable for mild to moderate sleep apnoea.
It can be performed using traditional surgical techniques or laser-assisted (as an outpatient). Some studies show it produced a 50 per cent reduction in breathing interruptions in 80 per cent of cases, but it often does not offer a total cure.
Risks: Post-operative bleeding and infection.
Somnoplasty: Low-intensity radiowaves are blasted at the soft palate tissues, which stiffens them so they vibrate less. Effective for people with mild to moderate sleep apnoea.
‘This can improve snoring in four out of five cases, but may require several treatments,’ says Mr Frosh.
Risks: While less invasive and painful than a UPPP, repeat treatments are usually needed.
Palatal stiffening: Radiofrequency heat is targeted at underlying muscles in the soft palate, causing them to stiffen. Tiny polyester beads are then inserted into the soft palate under local anaesthetic to reduce tissue vibration. It can be successful in patients with recurrent snoring problems or mild to moderate sleep apnoea.
Risks: Occasionally beads may become dislodged, so it may need to be repeated.
For growths and bent noses
Polyp removal: Nasal polyps are inflammatory swellings of the tissue lining the nose and can cause nasal obstruction and snoring. They can form as a result of an inflammatory disease or an allergy. This can sometimes be severe enough to tip a patient who simply snores into sleep apnoea.
Steroid nasal sprays (see previous page) can help to shrink polyps or reduce growth.
If not, they can be removed with a relatively low risk keyhole operation – which produces an 80 per cent reduction in symptoms.
Septoplasty: A deviated septum is where the strip of cartilage between the two nostrils is misaligned, often as a result of an anatomical defect from birth or caused by an injury. It can restrict the airway and cause snoring.
Surgery to realign the wall, known as septoplasty, can improve breathing and stop snoring as a secondary benefit.
Risks: Post-operative bleeding and infection.
Turbinate reduction: Turbinates are curved bony structures that protrude into the sides of the nasal cavity and usually direct the airflow.
Problems can be sporadic (e.g. worsened by seasonal allergies), but if swollen they can reduce breathing and surgery may be required to reduce their size.
Risks: Post-operative bleeding and infection (both rare). Also ’empty nose’ syndrome, where the reduced resistance in the nasal passages leads the patient to feel they can’t inhale properly.
‘I’m now more positive and less anxious’
Feras Nasser, 47 , a business psychologist, lives in Hitchin, Herts, with his wife Achsah, 42, who works in banking, and their daughter, 11, and son, eight. He says: I’ve been a heavy snorer for as long as I can recall. I was the teenager nobody wanted to share a bedroom with on school trips. At 19, I even kept people in other tents awake at Glastonbury!
Drinking less alcohol and losing weight helped a bit as a young man – but I’m still quite a big man; about 4 st 10 lb (30kg) over my ideal weight.

Feras Nasser, 47, suffers from sleep apnoea but no longer snores, thanks to the CPAP machine
It really affected my life; I was always exhausted and felt low. Once I even missed picking up my son from school, as I’d fallen asleep on the sofa. I put this down to pressures of running a successful business and juggling a family – until two years ago when a friend mentioned her husband had sleep apnoea. His symptoms sounded just like mine.
My GP referred me for tests and it turned out I had huge tonsils – they were the highest rating on a size chart and were nearly blocking the back of my throat, especially while asleep.
A sleep apnoea test – I wore a device to measure my blood oxygen levels and breathing for two nights – showed that my throat was being blocked off 73 times an hour (with a normal person this is less than five).
I used my health insurance to have my tonsils removed, and my uvula [the soft hanging ball at the back of my throat] trimmed, to widen my airway, under general anaesthetic.
The next two weeks were tough – my throat was raw. I also started using a CPAP machine: it took a while to get used to, but it has been life-changing.
I no longer snore, I wake full of energy and I’ve taken up mountain biking with my kids. I’m also more positive and much less anxious.